How Does the ACA Expansion Affect Medicaid Coverage Before and During Pregnancy?
By Bradley Corallo and Brittni Frederiksen / October 26, 2022
Medicaid is a major source of coverage for pregnant women, financing roughly four in ten births nationally and a majority in some states. A recent report on maternal health found that more than 80% of pregnancy-related deaths were preventable and recommended broader access to health insurance, which can improve prenatal care initiation and follow-up after pregnancy. A previous KFF analysis found that postpartum enrollees in Medicaid expansion states had greater continuity of Medicaid coverage in the year following childbirth, compared to enrollees in non-expansion states. However, the analysis did not examine coverage in the months leading up to childbirth. Coverage prior to and throughout pregnancy can promote pre-pregnancy health care and early prenatal care, including many of the services and tests provided during the first trimester, which can lead to healthier pregnancies and help reduce the risk of complications. In this brief, we examine whether the Medicaid expansion also helps women enroll earlier in the months leading up to pregnancy and childbirth using Medicaid claims data for women with a live birth in 2019.
Women in expansion states are more than twice as likely to be enrolled in Medicaid prior to becoming pregnant compared to women in non-expansion states (Figure 1). Most (59%) enrollees in expansion states with a live birth were enrolled prior to pregnancy (at least 11 months before delivery), while only 26% of enrollees in non-expansion states were enrolled prior to pregnancy. Four in ten (40%) enrollees with a live birth in non-expansion states enrolled once they became pregnant or soon after (7-10 months prior to delivery). Generally, the income limits for pregnant women to qualify for Medicaid coverage are higher than the limits for other adults, which allow many women to become newly eligible for Medicaid once they are pregnant. The difference in income levels between pregnant adults and other adults is especially large in non-expansion states (Appendix Table 1), which helps to explain why a smaller share of women in these states are enrolled in Medicaid prior to the start of pregnancy. Other research has found that most of the women newly enrolled in Medicaid during their pregnancy were uninsured before enrolling, and the rate of uninsured women who gain pregnancy-related Medicaid coverage is higher in non-expansion states.
Women in non-expansion states are more likely to enroll later in their pregnancy than women in expansion states. About one-third (34%) of pregnant women in non-expansion states enrolled in Medicaid within six months of delivery, roughly in the second trimester or later in their pregnancy, compared to 22% of women in expansion states. Smaller shares of women enrolling in Medicaid during the month of delivery could have been uninsured at the time of delivery but were found to be eligible during their hospital stay.
Our analysis of prenatal coverage in Medicaid builds on previous KFF research, which together find that the Medicaid expansion promotes continuity of coverage in the prenatal and postpartum periods. Other research also finds that expansion has contributed to improvements in a number of outcomes related to reproductive health. Looking ahead, the Medicaid expansion may be a key issue in several state elections. In the 12 states that have not adopted the Medicaid expansion as of 2022, all but two (North Carolina and Mississippi) have upcoming gubernatorial elections in November 2022. Additionally, South Dakotans will vote on a ballot measure to enact the Medicaid expansion through a constitutional amendment. If passed, the amendment would direct the state to implement the Medicaid expansion by July 1, 2023. In North Carolina, state legislators may renew discussions on the Medicaid expansion, which passed in separate bills in both state legislative bodies but was not included in the final FY 2023 budget bill. States that newly implement Medicaid expansion will receive a temporary fiscal incentive under the American Rescue Plan Act through an enhanced federal match on most Medicaid spending. The outcome of the recent court decision overturning Roe v. Wade has highlighted the importance of health coverage for women and children, especially those with low incomes.
Methods
Data Source and Sample Selection
Our analysis uses the Transformed Medicaid Statistical Information System (T-MSIS) Analytic Files (TAF) Research Identifiable Files (RIF), 2018 – 2019, Release 1. We linked the 2019 Inpatient and Other Services header files with the 2018-2019 Demographic Eligibility (DE) Base File and DE Dates File. We used BENE_ID to link files when available and, when BENE_ID was missing, we used MSIS_ID to link files (see the TMSIS User Guide for information on linking variables).
To identify Medicaid enrollees with a live birth in 2019, we use the reference codes for live births provided by Calkins et al. in their technical specifications for “Maternal and Infant Health (MIH): Identifying Pregnant and Postpartum Beneficiaries in Administrative Data,” available on the CMS website. After flagging patients with a live birth in 2019 in the claims files we merged the claims file with the eligibility files and excluded individuals enrolled through a medically needy eligibility pathway or through a separate Children’s Health Insurance Program (SCHIP) during the month of delivery. Finally, we measured the length of time women were continuously enrolled leading up to childbirth. If enrollees had a gap in coverage that was 27 days or less (less than one month) then we considered that person to be continuously enrolled from before the gap in prenatal coverage. If an enrollee had a gap in coverage during the prenatal period that was 28 days or more, we only included the latest enrollment period following the gap and leading up to childbirth. However, we expect very few pregnant women to have gaps in coverage because the federal government requires that pregnant enrollees have continuous eligibility from the month of application for Medicaid through at least 60 days postpartum.
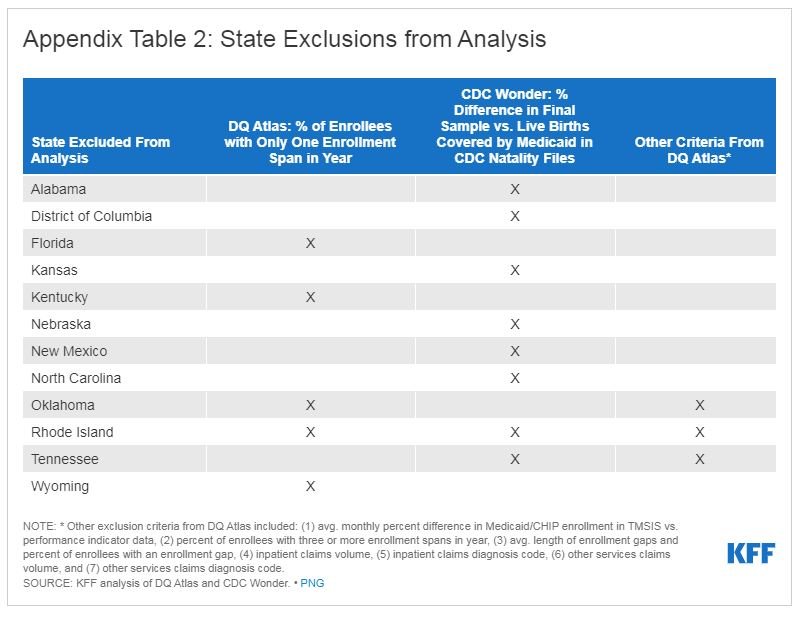
State Exclusion Criteria
We use data from 39 states in our analysis. We exclude 12 states (AL, DC, FL, KS, KY, NC, NE, NM, OK, RI, TN, and WY) due to missing or inconsistent data based on state-level information available from the DQ Atlas as well as our own analysis of the CDC Wonder Natality Files. We used several measures from the DQ Atlas to assess states’ data quality, shown in Appendix Table 2. We further excluded states whose final sample in this analysis had a difference of 20% or more from the number of Medicaid-covered births in the CDC Wonder Natality Files. In total, our final sample included 1,259,397 deduplicated enrollees with a live birth, while CDC Wonder reported 1,254,767 newborns covered by Medicaid (a difference of +0.4% from CDC Wonder).