What Does the Recent Literature Say About Medicaid Expansion?: Economic Impacts on Providers
By Meghana Ammula and Madeline Guth / January 18, 2023
A substantial body of research has investigated effects of the Affordable Care Act (ACA) Medicaid expansion, adopted by all but 11 states as of January 2023. Prior KFF reports published in 2020 and 2021 reviewed more than 600 studies and concluded that expansion is linked to gains in coverage, improvement in access and health, and economic benefits for states and providers; these generally positive findings persist even as more recent research considers increasingly complex and specific outcomes. This research provides context for ongoing debates about whether to expand Medicaid in states that have not done so already, where coverage options for many low-income adults are limited. In non-expansion states, over two million individuals fall into a coverage gap. Prior efforts at the federal level to temporarily close the coverage gap were unsuccessful in 2021 and 2022, and Republican control of the House of Representatives following the November 2022 midterm elections makes it highly unlikely that Congress will do so in the near future. So, attention once again turns back to non-expansion states, where many officials cite economic concerns about adopting Medicaid expansion.
While states have to cover 10% of the cost of expanding Medicaid, the federal government covers the remaining 90%, providing an infusion of federal funds to expansion states. By financing coverage for low-income people who are likely to otherwise be uninsured, Medicaid expansion provides potential economic benefits to the health care providers who provide care to that population.
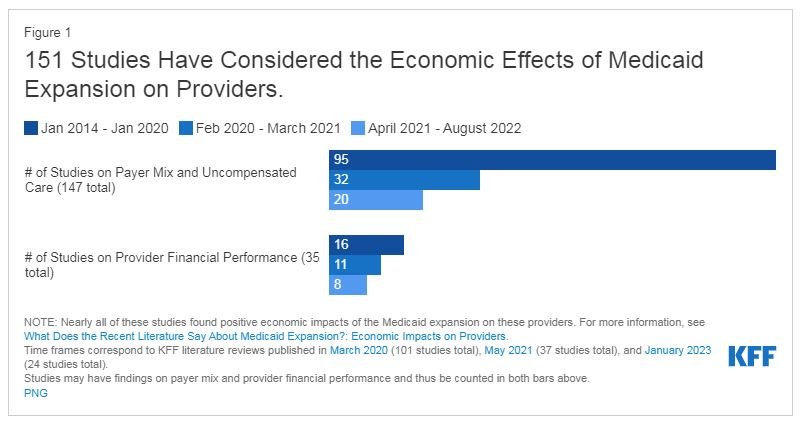
This issue brief updates prior KFF literature reviews by summarizing 24 studies published between April 2021 and December 2022 on the economic impact of Medicaid expansion on providers. These studies identify positive effects of Medicaid expansion on the finances of hospitals and other providers, in line with prior research. These findings are particularly relevant given fiscal stress experienced by Medicaid providers during the coronavirus pandemic. While federal relief funds helped prop up hospital margins in the first two years of the pandemic, hospitals began facing increased challenges in 2022 due to ongoing pandemic effects, decreases in government relief, and broader economic trends such as pressure on wages.
Our methodology is consistent with that of prior analyses. Study findings fall into two topic areas: impacts on payer mix and on the financial performance of providers (Figure 1). Within each topic area, we first briefly summarize findings from earlier research (published between January 2014 and March 2021) and then highlight key findings from recent research that add to this body of evidence. For more information about earlier studies, see the 2021 and 2020 literature review sections on the economic impacts on providers. For citations from January 2014 through August 2022, see the Bibliography.
Payer Mix and Uncompensated Care
Prior studies overwhelmingly found that Medicaid expansion has resulted in payer mix improvements (declines in uninsured patients and/or increases in Medicaid-covered patients). Findings include payer mix improvements for hospitalizations, emergency department visits, and visits to community health centers and other safety-net clinics. Studies identify payer mix improvements overall and among patients being treated for a range of specific conditions, including different types of cancer, traumatic injuries, and substance use disorder. In line with payer mix improvements, studies also find decreased uncompensated care costs (UCC) overall and for specific types of hospitals, including those in rural areas.
Consistent with previous research, nearly all recent studies find that expansion has resulted in payer mix improvements, including among patients treated for specific conditions, as well as decreases in UCC. Of eighteen studies that consider the impact of expansion on payer mix, eleven find both decreases in the proportion of uninsured patients and increases in Medicaid-covered patients,1,2,3,4,5,6,7,8,9,10,11 and an additional five studies find increases in Medicaid patients but did not study or found no impact of expansion on the proportion of uninsured patients.12,13,14,15,16,17 In line with these improvements, three studies also find decreased UCC for hospitals and other providers.18,19,20 Notably, all studies that considered emergency department visits found payer mix improvements. Studies continue to consider and find payer mix improvements for patients treated for specific conditions, such as different types of surgery and behavioral health admissions. Although studies evaluating payer mix most frequently consider hospitals, two recent studies considered coverage of primary care patients; both found that Medicaid-covered visits to primary care providers increased.21,22,23 Just two recent studies found no impact of expansion on payer mix but were narrowly focused on critical access and safety-net provider.24,25
Financial Performance of Hospitals and Other Providers
Prior research found that Medicaid expansion has improved the financial performance of hospitals and other providers, though these effects may vary somewhat by hospital type. Studies show that expansion contributed to increased hospital revenue overall and from specific services. A few studies indicate that expansion reduced the number of annual hospital closures. Although studies find that expansion has improved provider operating margins and profitability, these findings vary by provider type. For example, a few studies find that despite declines in UCC, improvements in financial performance were stronger for (or only observed among) rural and small hospitals. A small number of studies suggest that improvements in payer mix and UCC at hospitals may have been partially offset by increases in unreimbursed Medicaid care and declines in commercial revenue.
Recent studies continue to find mostly positive financial impacts of expansion on specific types of hospitals, clinics, and other providers. Of eight studies in this area, six find that expansion resulted in positive financial outcomes for a range of provider types,26,27,28,29,30,31 while two recent studies suggest that these positive effects did not extend to critical access hospitals or free and charitable clinics.32,33
Hospitals. Studies suggest that hospitals experienced higher reimbursements and that decreased uncompensated care costs outweighed increases in unreimbursed Medicaid care for a net positive effect.34,35 One study found that expansion was associated with a large reduction in hospital closures, but that this effect was concentrated among hospitals without obstetrics units, while expansion had no lasting effects on closures of hospital-based obstetrics units.36 Federal law requires all states, including those that have not expanded Medicaid, to provide Medicaid coverage to pregnant women with incomes up to at least 138% of the poverty level.37
Clinics and primary care providers. Studies find that federally qualified health centers and community health centers experienced increased revenue following expansion.38,39 Also, one study found higher salary growth for primary care providers in expansion versus non-expansion states.41
Looking Ahead
These new studies add to the body of prior research finding overwhelmingly positive economic effects of expansion on providers. Such findings are particularly relevant given the fiscal stress experienced by Medicaid providers during the coronavirus pandemic, including recent challenges faced by hospitals as federal relief funds expire. This research also provides context for ongoing debates about whether to expand Medicaid in states that have not done so already. Additionally, earlier literature on the financial impact of expansion on states found positive effects, including budget savings, revenue gains, and overall economic growth. Although research in this area appears to have slowed, these findings remain relevant: state costs continue to be a key issue in expansion debates and there have been fluctuations in state economic conditions during the COVID-19 pandemic. Future research could also capture the effect of the additional temporary fiscal incentive included in the American Rescue Plan Act (ARPA) of 2021 (estimated to more than offset the state costs of expansion for the first two years following implementation).41