Up to 80,000 Ohioans could end up on different health plan in reformed Medicaid system
Titus Wu / The Columbus Dispatch
You probably don't want to ever find yourself surprised during a doctor's visit that your health plan was automatically changed. So if you're currently receiving health care through Medicaid in Ohio, you should make sure you actively choose your plan.
The Ohio Department of Medicaid finalized enrollment details Friday for its rollout of a revamped and reformed Medicaid managed care system set to begin July. Part of that may include transferring up to 80,000 Ohioans to a different plan at the end of the year.
Medicaid, the state- and federally-paid health insurance for nearly 3 million disabled and/or low-income Ohioans, is typically the state's largest expenditure totaling billions of dollars. The taxpayer money under managed care is doled out to contracted private health plans which provide the coverage.
The planned reforms come after years of various issues. The requirement of active re-enrollment is one of those reforms, as well as a result of new contractees competing for members.
Sticking to the same plan?
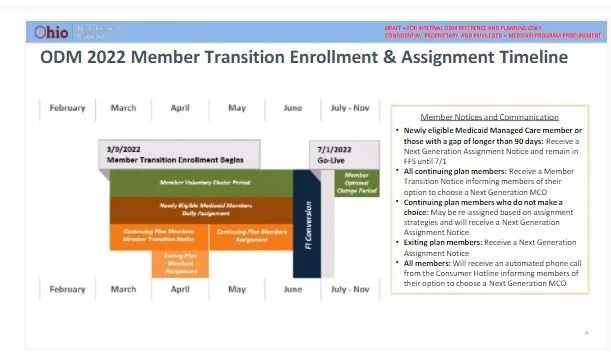
New and current Medicaid participants will receive a notice asking them to actively choose a plan. From early March to June, one can choose to remain in the same plan or select a different one.
That's different from before when individuals were automatically put back in the same plan. The change is to nudge people into knowing about their own health plan, and in turn, health outcomes would be improved.
"There were people on the program who didn't even realize some of those simple things… about transportation being available to your doctor, or that your management people can help coordinate your care," Ohio Medicaid Director Maureen Corcoran previously said.
But there was criticism that Medicaid recipients, who tend to be difficult to reach and in disadvantaged communities, are less likely to actively enroll. Advocates feared those who didn't make a choice would find themselves assigned to completely different plans, to their surprise.
New adjustments to the plan could erase those concerns. According to Corcoran, the top factors when assigning someone would be ensuring physicians and other providers remain mostly constant and all members of a family receive the same coverage.
As a result, nobody currently on Medicaid will be assigned to a different health plan, she emphasized – at least when the new system begins.
Additionally, the department is looking at a more aggressive outreach campaign to make people aware of the change. In the past, only around 20% actively chose a plan with communication mostly by mail, Corcoran had said.
Even under the worst-case scenario, one can still switch to a plan different from their assigned one until the end of November – much longer than the typical one-month period allowed for switches every year.
Who goes where?
All that emphasis on choice and no disruptions has to be balanced with the fact that every plan needs enough members to be financially viable. With the revamped system, contracts had to be redone, and this time, there are two more companies that are eyeing a share of Medicaid members to cover.
Buckeye Health Plan, CareSource, Molina Healthcare and UnitedHealthcare will continue on as options, while Paramount Advantage is set to be acquired by Anthem Blue Cross and Blue Shield. AmeriHealth Caritas and Humana will be completely new to Ohio's Medicaid system.
The state is obligated to spread around members among more companies. Financial stakes are huge, as plans get paid a certain amount of dollars per patient.
Corcoran said Ohio is planning to assign roughly 200,000 members to each of the new plans. But if all current members should be kept on the same plan, where will the new plans get their 200,000 customers?
The department plans to have almost all new Medicaid participants assigned to the new plans, Corcoran said. The rest will need to come from the more-easily-transferable "churn" population – members who lose Medicaid eligibility but come back after a while.
However, the COVID-19 pandemic caused the federal government to issue a public health emergency declaration, which is still active. It prevents anyone from being kicked off Medicaid.
If the declaration ends early, no action may be needed. But if it continues on, Corcoran said the state may need to shift 45,000 to 80,000 people to new plans after November to give the new plans financial viability.
Those targeted for transfers would be those at the least risk from changing health plans, such as people who rarely need medical care. But even then: they still can actively choose to go back to their current plan.
What happens if all that 80,000 refuses to switch? To be determined, Corcoran said. There are a lot of moving parts, but an enrollee's choice will always be honored.
"Consumers are going to be first; they're going to have the choice. They're not going to be disrupted," she said.
An internal document of enrollment plans can be viewed below. Note: Some details have changed since.