Medicaid Enrollment and Unwinding Tracker
By KFF / June 29, 2023
The Medicaid Enrollment and Unwinding Tracker presents the most recent data on monthly Medicaid enrollment, renewals, disenrollments, and other key indicators reported by states during the unwinding of the Medicaid continuous enrollment provision. The unwinding data are pulled from state websites, where available, and from the Centers for Medicare & Medicaid Services (CMS).
State Medicaid Disenrollment Data
At least 1,536,000 Medicaid enrollees have been disenrolled as of June 29, 2023, based on the most current data from 27 states and the District of Columbia. Overall, 38% of people with a completed renewal were disenrolled in reporting states while 62%, or 2.6 million enrollees, had their coverage renewed (four of the 27 reporting states do not provide data on renewed enrollees). Because not all states have publicly available data on total disenrollments, the data reported here undercount the actual number of disenrollments.
There is wide variation in disenrollment rates across reporting states, ranging from 75% in South Carolina to 16% in Virginia. Differences in who states are targeting with early renewals as well as differences in renewal policies and systems capacity likely explain some of the variation in disenrollment rates. Some states (such as South Carolina) are initially targeting people early in the unwinding period that they think are no longer eligible or who did not respond to renewal requests during the pandemic, but other states are conducting renewals based on an individual’s renewal date. Additionally, some states have adopted several policies that promote continued coverage among those who remain eligible and have automated eligibility systems that can more easily and accurately process renewals while other states have adopted fewer of these policies and have more manually-driven systems.
(Note: disenrollment rate calculations do not include renewals that are still pending. If these pending renewals, which are large in many states, were included, the disenrollment rates would be lower. For example, South Carolina’s disenrollment rate would drop from 75% to 47% if pending renewals in the state were included in the calculation. More detailed information on completed and pending renewals for states is available here.)
Across all states with available data, 71% of all people disenrolled had their coverage terminated for procedural reasons. There is also wide variation in rates of procedural disenrollments across states reporting this breakout, ranging from 93% in South Carolina to 15% in Alaska. Procedural disenrollments are cases where people are disenrolled because they did not complete the renewal process and can occur when the state has outdated contact information or because the enrollee does not understand or otherwise does not complete renewal packets within a specific timeframe. High procedural disenrollment rates are concerning because many people who are disenrolled for these paperwork reasons may still be eligible for Medicaid coverage.
(Note: procedural disenrollment rates are calculated using total disenrollments as the denominator. The number of people whose coverage was renewed as well as the number of pending renewals are not included in these calculations. Including these counts would lower the procedural disenrollment rates. For example, Nevada’s procedural disenrollment rate would drop from 70% to 41% if these counts were included in the calculation. More detailed information on completed and pending renewals for states is available here.)
Although data are limited, children accounted for over one-third (37%) of Medicaid disenrollments in five states reporting age breakouts. As of June 29, 2023, at least 156,000 children had been disenrolled out of 425,000 total disenrollments in the five states. The share of children disenrolled ranged from 39% in Arkansas to 32% in Oklahoma.
Background on the Unwinding of the Medicaid Continuous Enrollment Provision
The Medicaid continuous enrollment provision, which had halted Medicaid disenrollments since March 2020, ended on March 31, 2023. Primarily due to the continuous enrollment provision, KFF estimates that enrollment in Medicaid/CHIP grew by 23.3 million to nearly 95 million from February 2020 to the end of March 2023. As states unwind the continuous enrollment provision over the following 12 months, they will redetermine eligibility for all Medicaid enrollees and will disenroll those who are no longer eligible or who may remain eligible but are unable to complete the renewal process. Millions of people are expected to lose Medicaid coverage during this unwinding period.
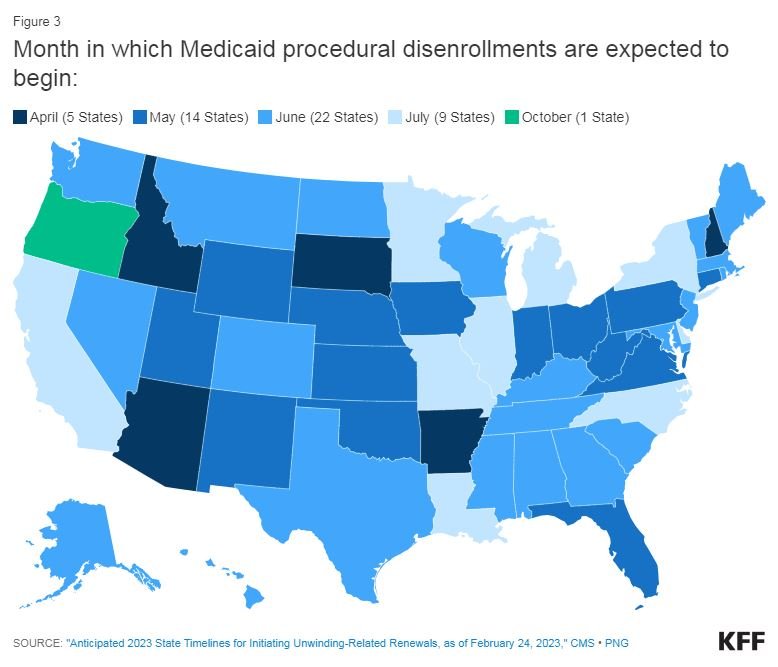
States will begin disenrolling people from Medicaid in different months, with some states resuming disenrollments in April, others in May or June, and even July or later for some states. The figure below shows the month in which disenrollments are expected to begin in each state.