Do State Decisions to Prioritize Renewals for Medicaid Enrollees Who are Likely Ineligible Affect Early Disenrollment Rates?
By Bradley Corallo, Jennifer Tolbert and Robin Rudowitz / August 11, 2023
As states resumed disenrolling people from Medicaid earlier this year as part of the “unwinding” of the continuous enrollment provision, early data have shown wide variation in disenrollment rates across states, ranging from 82% of completed renewals in Texas to 10% in Michigan. Although there are a range of state policy choices and other factors contributing to this variation, this policy watch examines which states are prioritizing renewals for enrollees that were flagged as likely ineligible and what effect that may have on disenrollment rates early in the unwinding period.
Prior to the start of the unwinding, many states flagged enrollees they deemed as likely ineligible. Although states could not disenroll anyone while the continuous enrollment provision, many states identified people as likely ineligible if there was information available showing the enrollee had a change in circumstance (e.g., aged out of children’s coverage), a change in income that would make them ineligible, or if they did not respond to renewal requests.
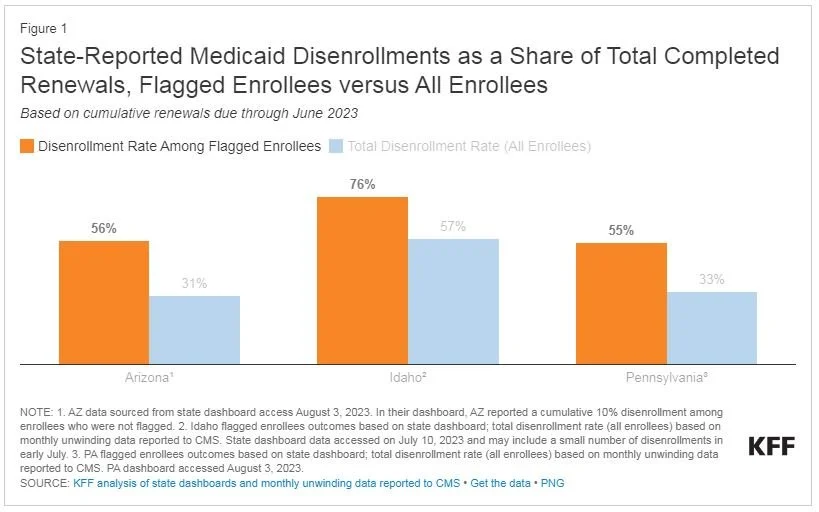
Early data from three states (Arizona, Idaho, and Pennsylvania) show that disenrollment rates for flagged enrollees are higher than for other enrollees. While several states publish total disenrollments among flagged enrollees, only Arizona, Idaho, and Pennsylvania publish enough information to be able to compare disenrollment rates for flagged enrollees to overall disenrollment rates. Based on early unwinding data, the disenrollment rate for flagged enrollees in each of these states exceeded the overall disenrollment rate by about 20 percentage points (Figure 1).
Some states are prioritizing renewals for enrollees flagged as likely ineligible early in the unwinding period. States have taken different approaches to processing renewals during the unwinding period and some states have chosen to prioritize renewals for enrollees they identified as likely no longer eligible during the first six months. Based on unwinding plans submitted to the Centers for Medicare and Medicaid Services (CMS), a total of 17 states indicated that they would prioritize renewals for enrollees that the state flagged as likely ineligible at the start of their unwinding period (Figure 2). Of these, 11 states plan to work through renewals for flagged enrollees during the first two-to-six months of the unwinding, while the remaining six states will spread renewals for flagged enrollees over the first seven-to-nine months.
State approaches to renewing flagged enrollees may explain some – but not all – variation in disenrollment rates across states. Consistent with the data from Arizona, Idaho, and Pennsylvania showing higher disenrollment rates for flagged enrollees, states that prioritize renewals for flagged enrollees in the first two-to-six months have a higher median disenrollment rate (48%) compared to all other states with available data (33%). However, there is still considerable variation in disenrollment rates among these states, ranging from 82% in Texas to 27% in Maryland (Figure 3). Some variation may reflect how states identified likely ineligible enrollees and the share of flagged enrollees undergoing a renewal each month. Other state policies likely contribute to the variation as well, such as the approach states take to increase the number of automatic (or ex parte) renewals, how states use temporary flexibilities made available by the federal government during the unwinding, and the effectiveness of states’ outreach to enrollees.
For states prioritizing likely ineligible enrollees, additional data may be required to identify potential reasons for high Medicaid disenrollments. Generally, states that heavily frontload renewals with flagged enrollees can be expected to have higher early disenrollment rates relative to states that spread out renewals for flagged enrollees over a longer period. But, over time, as these states work through renewals for flagged enrollees, disenrollment rates should moderate. However, if these higher disenrollment rates are because of other issues with a state’s renewal process, waiting several months to see whether disenrollment rates decrease could mean many eligible enrollees may lose coverage. More complete information on the reasons why individuals were flagged as likely ineligible, the share of flagged enrollees being renewed each month, as well as disenrollment data broken out by flagged enrollees versus all other enrollees could help identify the factors that underpin disenrollment rates early in the unwinding period.